INTERNATIONAL JOURNAL OF BIOMEDICINE Mammographic Density Errors during Interpretation of Breast Examinations
25 февраля 2021
INTERNATIONAL JOURNAL OF BIOMEDICINE
International Journal of Biomedicine 10(4) (2020) 378-381
ORIGINAL ARTICLE
Radiology
Mammographic Density Errors during Interpretation of Breast Examinations
Tamara V. Pavlova, MD, PhD1,2; Aleksandr Yu. Vasilyev, MD, PhD, ScD1,3*;
Ivan V. Buromsky, MD, PhD, ScD4
1Central Research Institute of Radiation Diagnostics
2City Clinical Hospital named after V. M. Buyanov
3Moscow State University of Medicine and Dentistry named after A. I. Evdokimov
4Russian National Research Medical University named after N. I. Pirogov
Moscow, Russia
Abstract
Background: This article discusses errors that may occur when radiologists deal with mammographic density (MD) and present their performance analysis in Russia. Methods and Results: The authors of this report have analyzed 24,485 mammographic reports for 20,000 female patients (aged 29-85 years) that were made in various healthcare facilities in the Russian Federation. In 249(1.7%) mammographic exam reports, we observed a wrong MD interpretation.
Conclusion: Diagnostic errors during mammographic examination occur because the radiologists lack theoretical knowledge about MD. This lack, in turn, results in a decrease in the quality of medical care provided for female patients and an increase in the number of diagnostic iatrogeny. (International Journal of Biomedicine. 2020;10(4):378-381.) Key Words: mammographic density • iatrogeny • error • breast cancer
Abbreviations
MD, mammographic density; BC, breast cancer.
Introduction
Despite the fact that medicine is constantly developing, and there are many scientific works devoted to the diagnosis and treatment of breast cancer (BC), the incidence and mortality rates of this disease are among the highest of all the cancer types.(1-3) Like any other pathologic process, a BC has its own risk factors. Many scientists believe that mammographic density (MD) is the key BC predictor.(4-6) Various sources state that according to the mammogram results, more than half of female patients under 50 have high MD values.(7) It is worth mentioning that the mammograms that display a high and extreme MD are often hard to interpret.(8) On the one hand, there is a risk of obtaining a false-negative result because the diagnostic accuracy of mammography decreases; on the other hand, a risk of a false-positive due to the tissue architecture superposition effect.(9,10) That is why the MD values are vital for determining the risk of breast cancer development. They should be under control throughout a patient’s life.(11) The scientists have proposed both quantitative and qualitative approaches to assessing MD, but the American College of Radiology (ACR) has strongly recommended using the latter one since 2013.(12-14) If MD is classified as “С” or “D,” the female patients are strongly recommended to undergo supplementary screenings; in most cases, this is an ultrasound scan, no matter whether they have pathologic changes or not.(15) However, due to certain subjectivity of classifications, there is some variability in mammographic pattern interpretation. This often results in miscategorization of MD and, consequently, in errors in further patient follow-up.
Materials and Methods
The authors of this report have analyzed 24,485 mammographic reports for 20,000 female patients (aged 29-85 years) that were made in various healthcare facilities in the Russian Federation in the period of 2008-2020, in order to assess the quality of work of Russian radiologists with regard to MD interpretation.
Results and Discussion
The MD category has been stated in 14,509(59.4%) cases. In 9,916 (40.6%) reports, there was no data about the MD category. If we speak about 14,509 cases, where the mammographic density has been stated, it is worth mentioning that in 6,645 (45.8%) cases the radiologists resorted to the outdated method of MD detection, which is based on the calculation of the percentage ratio of fat and fibroglandular components (Wolfe, 2003). Since 2013, the ACR has been taking into account the fact that the pathologic area can disguise itself as dense structures of a breast. Besides, Roman numerals (I-IV) that used to denote the MD grades were replaced by letters (A, B, C, D). As the research data embraced the period of 2008- 2020, we did not consider a percentage ratio method as a completely improper one. We have divided the mammographic reports into 2 groups, depending on the assessment systems for MD of breast tissue applied. The graph is shown in Fig. 1.
In 249 (1.7%) mammographic exam reports, we observed a wrong MD interpretation. The correlation between errors in MD detection and the total amount of categorized cases is shown in Fig.2.
Table 1 contains the cases of the wrong MD interpretations (249=100%).
We have divided them into the following categories:
1) 14 (5.6%) cases were classified as ACR BI-RADS А, while mammograms have shown that there is a sufficient amount of fibroglandular tissue.
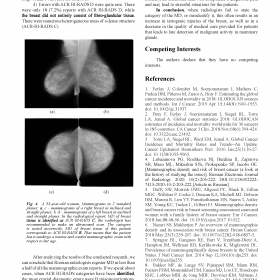
2) 151 (60.6%) cases were miscategorized as ACR BI-RADS B instead of А (n=104) or С (n=47) (Fig.3).
Fig. 1. The distribution of cases, depending on the employed method of evaluation and interpretation of MD (n=14,509)
Fig. 2. The error rate in MD of mammary gland tissue, if the density category is stated (n=14,509).
Table 1.
Fig. 3. A 49-year-old woman. Mammograms in 2 standard planes: а, c – mammograms of a right breast in inclined and straight planes; b, d – mammograms of a left breast in inclined and straight plane. In the radiological conclusion, MD of breast tissue is identified as ACR BI-RADS B; the female patient is supposed to undergo a mammographic exam one more time in 2 years. The category is stated incorrectly, MD of breast tissue of this patient corresponds to ACR BI-RADS С. That means that she should make an ultrasound scan immediately.
380 T. V. Pavlova et al. / International Journal of Biomedicine 10(4) (2020) 378-381
3) Heterogeneous MD (ACR BI-RADS C) was misinterpreted in 66 (26.5%) cases, while the exams of 52 female patients had to be interpreted as ACR BI-RADS B (Fig. 4) and 14 as ACR BI-RADS D.
4) Errors with ACR BI-RADS D were quite rare. There were only 18 (7.2%) reports with ACR BI-RADS D, while the breast did not entirely consist of fibro-glandular tissue. There were numerous heterogeneous areas of a dense structure (ACR-BI-RADS C).
After analyzing the results of the conducted research, we can conclude that Russian radiologists register MD in less than a half of all the mammographic exam reports. If we speak about cases, when ACR BI-RADS categories have been identified, the most crucial diagnostic errors were B miscategorizations, when actually there were heterogeneous dense structures, and incorrectly stated C category for breasts with sporadic areas of fibroglandular tissue. In the first case, the patients won’t undergo an ultrasonic scan, which is obligatory and indicated for patients with high and extreme MD, and this can result in false-negative diagnostic results. In the second case, on the contrary, an ultrasonic scan will complicate a diagnostic path and may lead to stressful situations for the patients.
In conclusion, when radiologists fail to state the category of the MD, or misidentify it, this often results in an increase in iatrogenic injuries of the breast, as well as in a decrease in the quality of medical care provided for patients that leads to late detection of malignant activity in mammary glands.
International Journal of Biomedicine 10(4) (2020) 378-381
ORIGINAL ARTICLE
Radiology
Mammographic Density Errors during Interpretation of Breast Examinations
Tamara V. Pavlova, MD, PhD1,2; Aleksandr Yu. Vasilyev, MD, PhD, ScD1,3*;
Ivan V. Buromsky, MD, PhD, ScD4
1Central Research Institute of Radiation Diagnostics
2City Clinical Hospital named after V. M. Buyanov
3Moscow State University of Medicine and Dentistry named after A. I. Evdokimov
4Russian National Research Medical University named after N. I. Pirogov
Moscow, Russia
Abstract
Background: This article discusses errors that may occur when radiologists deal with mammographic density (MD) and present their performance analysis in Russia. Methods and Results: The authors of this report have analyzed 24,485 mammographic reports for 20,000 female patients (aged 29-85 years) that were made in various healthcare facilities in the Russian Federation. In 249(1.7%) mammographic exam reports, we observed a wrong MD interpretation.
Conclusion: Diagnostic errors during mammographic examination occur because the radiologists lack theoretical knowledge about MD. This lack, in turn, results in a decrease in the quality of medical care provided for female patients and an increase in the number of diagnostic iatrogeny. (International Journal of Biomedicine. 2020;10(4):378-381.) Key Words: mammographic density • iatrogeny • error • breast cancer
Abbreviations
MD, mammographic density; BC, breast cancer.
Introduction
Despite the fact that medicine is constantly developing, and there are many scientific works devoted to the diagnosis and treatment of breast cancer (BC), the incidence and mortality rates of this disease are among the highest of all the cancer types.(1-3) Like any other pathologic process, a BC has its own risk factors. Many scientists believe that mammographic density (MD) is the key BC predictor.(4-6) Various sources state that according to the mammogram results, more than half of female patients under 50 have high MD values.(7) It is worth mentioning that the mammograms that display a high and extreme MD are often hard to interpret.(8) On the one hand, there is a risk of obtaining a false-negative result because the diagnostic accuracy of mammography decreases; on the other hand, a risk of a false-positive due to the tissue architecture superposition effect.(9,10) That is why the MD values are vital for determining the risk of breast cancer development. They should be under control throughout a patient’s life.(11) The scientists have proposed both quantitative and qualitative approaches to assessing MD, but the American College of Radiology (ACR) has strongly recommended using the latter one since 2013.(12-14) If MD is classified as “С” or “D,” the female patients are strongly recommended to undergo supplementary screenings; in most cases, this is an ultrasound scan, no matter whether they have pathologic changes or not.(15) However, due to certain subjectivity of classifications, there is some variability in mammographic pattern interpretation. This often results in miscategorization of MD and, consequently, in errors in further patient follow-up.
Materials and Methods
The authors of this report have analyzed 24,485 mammographic reports for 20,000 female patients (aged 29-85 years) that were made in various healthcare facilities in the Russian Federation in the period of 2008-2020, in order to assess the quality of work of Russian radiologists with regard to MD interpretation.
Results and Discussion
The MD category has been stated in 14,509(59.4%) cases. In 9,916 (40.6%) reports, there was no data about the MD category. If we speak about 14,509 cases, where the mammographic density has been stated, it is worth mentioning that in 6,645 (45.8%) cases the radiologists resorted to the outdated method of MD detection, which is based on the calculation of the percentage ratio of fat and fibroglandular components (Wolfe, 2003). Since 2013, the ACR has been taking into account the fact that the pathologic area can disguise itself as dense structures of a breast. Besides, Roman numerals (I-IV) that used to denote the MD grades were replaced by letters (A, B, C, D). As the research data embraced the period of 2008- 2020, we did not consider a percentage ratio method as a completely improper one. We have divided the mammographic reports into 2 groups, depending on the assessment systems for MD of breast tissue applied. The graph is shown in Fig. 1.
In 249 (1.7%) mammographic exam reports, we observed a wrong MD interpretation. The correlation between errors in MD detection and the total amount of categorized cases is shown in Fig.2.
Table 1 contains the cases of the wrong MD interpretations (249=100%).
We have divided them into the following categories:
1) 14 (5.6%) cases were classified as ACR BI-RADS А, while mammograms have shown that there is a sufficient amount of fibroglandular tissue.
2) 151 (60.6%) cases were miscategorized as ACR BI-RADS B instead of А (n=104) or С (n=47) (Fig.3).
Fig. 1. The distribution of cases, depending on the employed method of evaluation and interpretation of MD (n=14,509)
Fig. 2. The error rate in MD of mammary gland tissue, if the density category is stated (n=14,509).
Table 1.
Fig. 3. A 49-year-old woman. Mammograms in 2 standard planes: а, c – mammograms of a right breast in inclined and straight planes; b, d – mammograms of a left breast in inclined and straight plane. In the radiological conclusion, MD of breast tissue is identified as ACR BI-RADS B; the female patient is supposed to undergo a mammographic exam one more time in 2 years. The category is stated incorrectly, MD of breast tissue of this patient corresponds to ACR BI-RADS С. That means that she should make an ultrasound scan immediately.
380 T. V. Pavlova et al. / International Journal of Biomedicine 10(4) (2020) 378-381
3) Heterogeneous MD (ACR BI-RADS C) was misinterpreted in 66 (26.5%) cases, while the exams of 52 female patients had to be interpreted as ACR BI-RADS B (Fig. 4) and 14 as ACR BI-RADS D.
4) Errors with ACR BI-RADS D were quite rare. There were only 18 (7.2%) reports with ACR BI-RADS D, while the breast did not entirely consist of fibro-glandular tissue. There were numerous heterogeneous areas of a dense structure (ACR-BI-RADS C).
After analyzing the results of the conducted research, we can conclude that Russian radiologists register MD in less than a half of all the mammographic exam reports. If we speak about cases, when ACR BI-RADS categories have been identified, the most crucial diagnostic errors were B miscategorizations, when actually there were heterogeneous dense structures, and incorrectly stated C category for breasts with sporadic areas of fibroglandular tissue. In the first case, the patients won’t undergo an ultrasonic scan, which is obligatory and indicated for patients with high and extreme MD, and this can result in false-negative diagnostic results. In the second case, on the contrary, an ultrasonic scan will complicate a diagnostic path and may lead to stressful situations for the patients.
In conclusion, when radiologists fail to state the category of the MD, or misidentify it, this often results in an increase in iatrogenic injuries of the breast, as well as in a decrease in the quality of medical care provided for patients that leads to late detection of malignant activity in mammary glands.